The State of Medication Access
Perhaps more than ever before, patients face significant barriers when trying to access the medication they need to live healthier lives. To explore these barriers in-depth, we expanded the focus of our annual report. Beyond adoption of technology solutions, we set out to tell a larger story of medication access challenges in America.
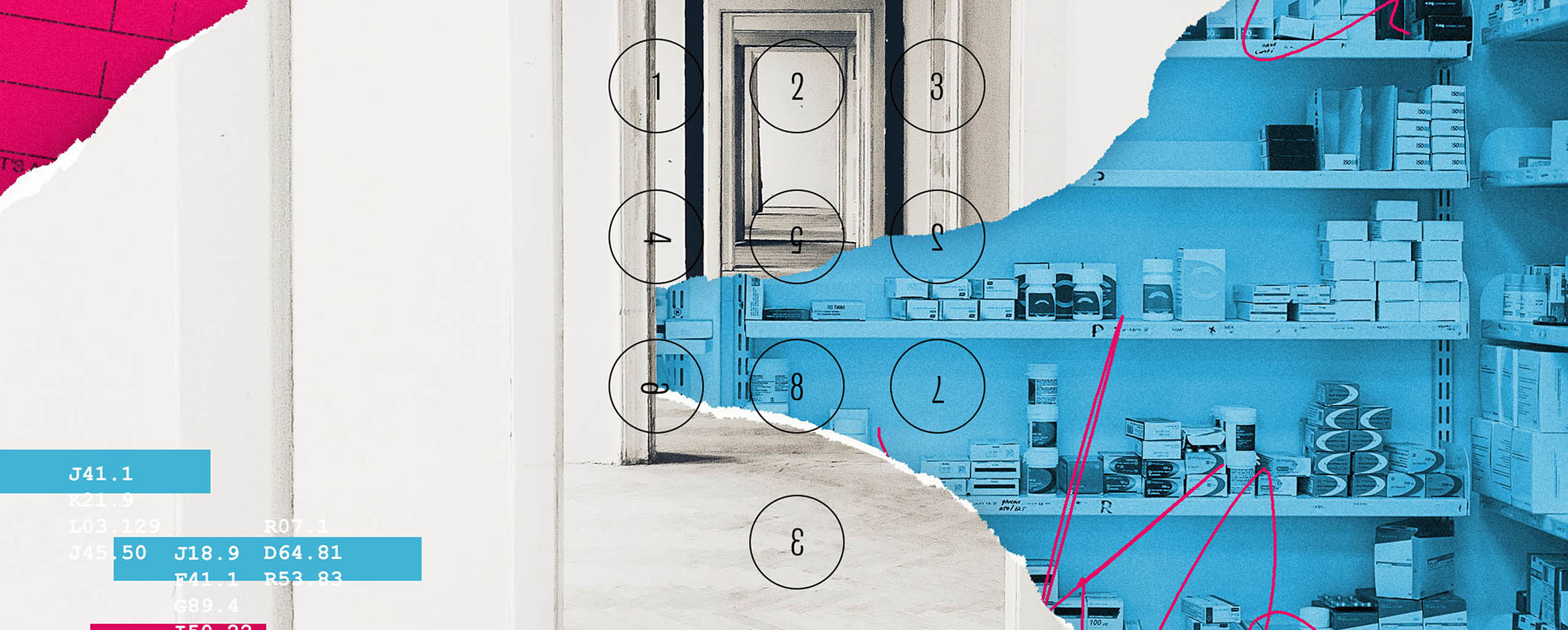
Earlier this year, we published our 2020 Medication Access Report — as well as supplemental reports focused on electronic prior authorization (ePA), prescription decision support and specialty patient support — in partnership with an advisory board of industry experts. This month, in light of the wide-ranging impact of the COVID-19 pandemic, we published an update on the state of medication access during these uncertain times.
The 2020 Medication Access Report examines what’s most important to both patients and providers now. Continue reading to explore key findings.
Please note: We’ve cited all data within the report, which you can access here.
Patients are also consumers
Nearly every industry has needed to adapt and evolve to meet consumers’ changing expectations — healthcare isn’t an exception. Notably, patients want more say in how they pay for their healthcare, therefore price transparency of prescription medications is increasingly important.
Three out of four survey respondents reported receiving a prescription that cost more than anticipated — and 50% admitted to leaving the pharmacy empty-handed because of this.
In the same survey, 69% reported that they’ve made personal or financial sacrifices to afford these medications — with more than one third making this tough decision every month.
Furthermore, 77% of those surveyed said it’s important or very important to proactively talk about affordability options with their doctor.
Empowering patients as educated consumers in their healthcare decisions can help to ease the economic pressures burdening so many. Affordability options for patients and prescription price transparency tools, like real-time benefit check, may help mitigate the challenges exacerbated by rising out-of-pocket spending.
As tech evolves, providers should continue to embrace ePA
One medication access barrier that remains top-of-mind for all stakeholders in a patient’s journey is prior authorization (PA), the process used by payers and PBMs to make coverage determinations and verify clinical decisions and make clinically appropriate coverage determinations.
Though a prescription can require PA for a few reasons, formulary exclusion is the most frequent — from 2014 to 2020, the number of medications added to the formulary exclusion lists for several large PBMs increased more than 500%.
According to the 2020 Medication Access Report, 76% of providers reported that they’ve switched a prescribed medication to avoid PA. Yet, nearly one third of patients surveyed expressed their preference to stay on their providers’ first choice of therapy even if it’s no longer covered — and 55% of patients reported experiencing a delay in accessing their prescription medication while waiting for PA request approval.
These findings reiterate much of what we already know — continued adoption of an electronic prior authorization (ePA) solution is essential. Allowing for real-time PA approvals, ePA can result in patients accessing their medications with little or no delay.
In the short-term, ePA allows pharmacies to easily start PA requests for providers to complete — mitigating challenges associated with excessive retrospective PA volume. In some cases, intelligent ePA technology can even recognize when a prescription requires PA and automatically start the request electronically. In the long-term, ePA enables a strategy to divert retrospective PA volume at the pharmacy to the point of prescribing — prospective ePA — in combination with prescription decision support tools, like real-time benefit check.
Patients need next-level support for specialty meds
More complex and more expensive, specialty medications pose unique — and significant — access barriers to patients. Clinical requirements, enrollment, coverage challenges and reimbursement are often impossible for a patient to navigate on their own. This process can result in prescription abandonment, delays in time to therapy and declining healthcare outcomes.
The 2020 Medication Access Report uncovers more details regarding the patient experience while accessing specialty therapies: Of more than 500 specialty patients surveyed, 60% claimed that they had some difficulty in receiving their first dose of specialty therapy, and 76% reported their personal role in coordinating care activities as involved or very involved. Patient support services (i.e., hubs) offered by manufacturers or third-party vendors are designed to guide patients through these challenges, but many patients are still unaware these services are available to them.
While one study of nearly 11,000 patients on a specialty medication recorded a 72% decrease in risk for therapy discontinuation for patients enrolled in a support program, another study of 10,000 patients found that as few as one in five patients were aware of these support programs.
Transitioning from the manual hub model to a technology platform already connected with major network stakeholders, a new patient support solution can now electronically complete more steps within the specialty workflow.
Through such an approach, established network connections give access to an active user base that can be transitioned to the new technology for specialty medication access.
The latest healthcare insights, floated right to your inbox.





